How to Store Breast Milk
There’s a reason parents call breast milk “liquid gold” for babies: it’s chock-full of nutrients, immune-boosting antibodies, good-for-the-gut bacteria, and enzymes that aid in digestion. For new Moms, safe storage guidelines for breast milk can be confusing—but knowing how to store breast milk properly is important. We’ve rounded up everything you need to know to ensure not a single drop of that liquid gold goes to waste.
How Long Should You Breastfeed?
The American Academy of Pediatrics (AAP) has historically recommended exclusive breastfeeding for the first six months of your baby’s life. In 2022, the AAP updated its breastfeeding recommendations to include extended breastfeeding beyond the first year:
“Updated AAP guidance continues to recommend exclusive breastfeeding for six months, with complementary foods introduced around six months. Under the new policy, the AAP now supports continued breastfeeding until two years or beyond, as mutually desired by mother and child.”
The World Health Organization (WHO) and the United Nations Children’s Fund (UNICEF) also recommend extended breastfeeding up to age two and beyond as the optimal feeding practice. Research has consistently demonstrated that extended breastfeeding benefits your toddler’s general health, nutrition, and cognitive and social development.
Will You Need a Breast Pump?
Not every new mom will need a breast pump, but most use one eventually, if only to take a (well-deserved) break from breastfeeding. You may need a breast pump if:
- Your baby is having trouble nursing—or isn’t nursing at all—and you need to maintain your milk supply.
- You plan to return to work part- or full-time and would like to continue feeding your baby breast milk.
- You’d like your baby to be fed breast milk exclusively but would want other caregivers to be able to participate in feedings.
- You’d like to be able to go out without your baby for more than a few hours at a time.
If you are staying home with your baby, are breastfeeding on demand, and your baby is gaining the appropriate amount of weight, you may not need an electric breast pump. A manual breast pump may be adequate for managing engorgement or increasing your supply.
Breast Milk Storage Guidelines
The Centers for Disease Control (CDC) has created guidelines for the safe storage of breast milk, but also note—significantly—that various factors, like milk volume, the room temperature where you’re pumping, temperature fluctuations in your fridge or freezer, and cleanliness of the pumping environment can affect how long you can safely store breast milk.
These guidelines are intended for mothers of full-term infants with no health complications. Use more conservative guidelines if your baby is preterm, in the NICU, or is otherwise ill.
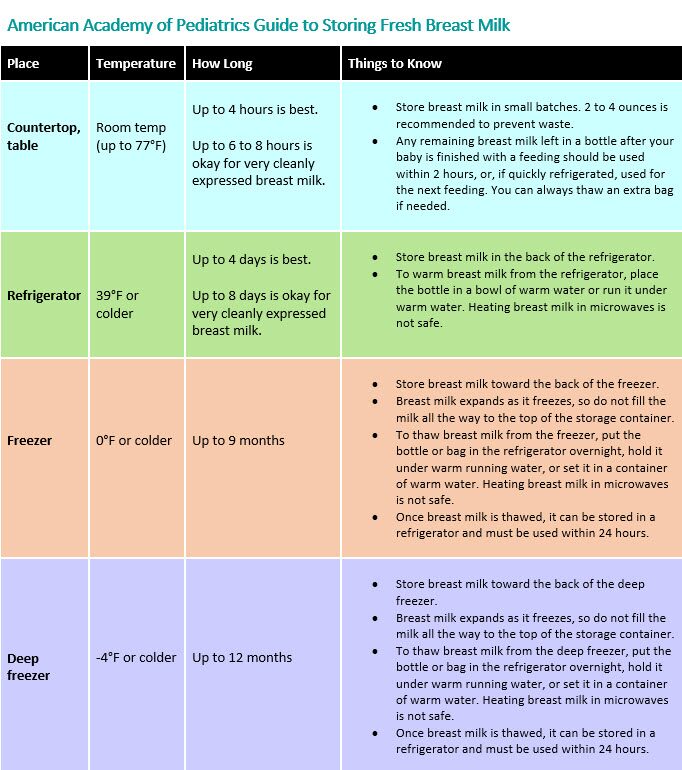
If your pregnant or postpartum brain is reeling, the AAP has a handy tip for remembering safe storage rules. Just follow their “rule of fours”: Breast milk can be safely stored at room temperature for four hours and in the fridge for four days.
How Can You Store Breast Milk?
You have a few options for safe breast milk storage. They recommend storing breast milk in breast milk storage bags or clean food-grade containers with tight-fitting lids. Avoid any plastic marked with the recycle symbols #3 or #7, indicating that the plastic contains BPA. (Polypropylene plastic, marked with the recycle symbol #3, is a safer alternative.)
There are three kinds of containers for safe breast milk storage, including breast milk storage bags, bottles, and breast milk storage trays (for freezing):
- Reusable silicone breast milk storage bags are an eco-friendly alternative to plastic storage bags. But they are more expensive and will need to be cleaned between uses.
- Pre-sterilized plastic breast milk storage bags are inexpensive, compact, and disposable. They also can be frozen in a flat package, clearing up freezer space. But they’re also a less eco-friendly option.
- If you’re using a pump, most come with glass or plastic bottles that you can pump into directly. While eco-friendly and convenient, it can get expensive if you’re pumping frequently.
- Breast milk storage trays are basically ice cube trays for your breast milk, and each portion typically holds an ounce of milk. They’re a convenient option, allowing you to thaw the exact amount of milk you need, but not the best option for storing a large amount of breast milk.
Use waterproof labels to label each container with the date you expressed the milk (the “first in, first out” rule applies here—you’ll want to use the oldest stored milk first).
General Breast Milk Storage Tips
- Breast milk should be refrigerated or frozen as soon as it’s expressed, preferably.
- Storing milk in 2-4 ounce amounts may help reduce waste, especially for newborns who don’t consume more than four ounces at each feeding.
- Refrigerated milk has less fat loss and more antibacterial protective properties than frozen milk.
- Always label your breast milk storage containers with the date you expressed the milk.
- Always use the oldest breast milk first.
- Squeeze any excess air out of breast milk storage bags before sealing them.
- If your baby will attend daycare or other childcare outside your home, include your baby’s name (along with the date).
- The CDC advises against mixing warm breast milk with milk that has been previously cooled—cool freshly expressed milk before combining it with milk that has been refrigerated or is frozen.
How to Store Breast Milk in the Refrigerator
CDC guidelines state that freshly expressed breast milk can be stored in the refrigerator for up to four days (though it’s optimal to either use or freeze refrigerated expressed milk within three days). Thawed breast milk should be used within twenty-four hours (start the countdown once the milk is thawed, not when you first take it out of the freezer).
Milk should be stored in the back of the refrigerator, where it’s the coolest. Never store breast milk in your refrigerator door—the door being opened and shut all day may make the milk too warm.
Once you’ve thawed breast milk, it should be used within twenty-four hours and should never be refrozen.
How to Store Breast Milk in the Freezer
Per the CDC, breast milk can be frozen for up to twelve months, but using frozen milk within six is ideal (the longer your milk is frozen, the more its nutritional qualities diminish). Again, milk should be stored in the back of the freezer, where it’s coolest, and never in the freezer door.
Because breast milk expands when it’s frozen, never fill a storage bag beyond the maximum fill level (generally six ounces). Leave an inch of space at the top if you’re using a different container for storage.
How to Store Breast Milk at Work
Pumping success at work relies on the right equipment, so make sure you pack a breast pump bag properly.
Freshly expressed milk can be stored in an insulated cooler with ice packs for up to twenty-four hours. At-work storage options include:
- If you have access to a refrigerator, store as you would home in storage bags, bottles, or other containers (it may be helpful to use a lunch bag to wrangle them in one space and prevent anything from being knocked over).
- Store in an insulated cooler bag with ice or freezable gel packs. We love the PackIt for this job—it’s lined on all sides with built-in freezable gel, so you don’t have to worry about adding ice cubes or additional ice packs.
How to Thaw Breast Milk
Remember, you always want to use your oldest breast milk first to preserve as many nutrients as possible (that’s why labeling is so important). You can safely thaw your breast milk by:
- Leaving it in the refrigerator overnight (remember, you’ll want to use it, once thawed, within twenty-four hours).
- Placing it in a container of warm water.
- Holding it under lukewarm running water.
Once breast milk is warmed or comes to room temperature, you’ll want to use it within two hours. Additionally, never thaw or heat breast milk in the microwave. Not only will the heat destroy nutrients, it can also create hot spots that can burn your little one’s mouth.
How to Feed Your Baby Expressed Breast Milk
Some good news: Warming and feeding your baby breast milk is (thankfully) uncomplicated. In fact, breast milk doesn’t need to be warmed at all—you can feed your baby cold milk if they don’t mind! If you do want to reheat your breast milk, the CDC has a few tips:
- Keep the milk in its sealed container or bag, and place it in a bowl of warm water or run it under a lukewarm tap.
- Check the temperature before feeding your baby (just dab a few drops on your wrist).
- Do not heat breast milk in the microwave or directly on the stove.
- You can reheat breast milk in a bottle warmer with a breast milk setting.
If your baby doesn’t finish their bottle, you can use the breast milk for another two hours. After that, you’ll need to toss it.
Breast Milk Storage FAQs
Why Is Your Milk Separating?
Breast milk will naturally separate into layers while being stored (you’ll see a milky bottom layer and a cream layer on top). Just shake, mix, or swirl to combine the cream before you feed your baby.
What If Your Power Goes Out?
Panicking is understandable if you have a freezer full of breast milk and wake up to a blinking clock and zero power. But take a few calming breaths because your milk will remain safe for your baby, probably for longer than you’re imagining.
According to CDC guidelines, breast milk stored in a full, unopened freezer is kept safe for up to forty-eight hours (and about twenty-four hours if half full). Why? A full freezer has more frozen items, keeping items colder for longer.
If left unopened, your fridge will keep breast milk safe for four hours. What’s the main message here? Try to avoid opening your freezer or fridge during a power outage. Once power is restored, check your breast milk. It can be refrozen if it’s thawing but still contains ice crystals. If it’s completely thawed but still cool, you can move it to the fridge—just make sure to use it within the next twenty-four hours (and throw it away if you don’t).
Can You Fly with Breast Milk?
Your breast milk can be safely stored in an insulated cooler for up to twenty-four hours, is considered “medically necessary” by the Transportation Security Administration (TSA), and does not need to fit within a quart-sized bag.
Let your TSA agent know you’re traveling with breast milk, and they can screen your cooler separately from your carry-on. Storing your breast milk in clear storage bags will help speed up the process.
Why Does Your Milk Smell or Taste Soapy?
Your thawed milk can look, smell, and taste differently than freshly expressed milk, and if you detect a soapy smell or taste, high lipase activity is the likely culprit. Lipases are enzymes found in all breast milk, and they do not indicate the milk is unsafe for your baby to drink.
And while it may be perfectly fine to drink, your baby may have their own opinions. If your baby rejects the milk, the La Leche League recommends mixing the thawed milk with cooled, freshly expressed milk.
Is It Safe to Store Milk in a Shared Refrigerator?
Yes! We recommend keeping your expressed milk in a cooler to prevent spills and ensure proper cooling on the way home. Again, ensure you’re storing your milk in the back of the refrigerator.
Is Your Milk Safe for Your Baby if You Have Thrush?
Thrush is an overgrowth of yeast that can cause an infection in your nipple or breast while nursing. If you’re worried that means you won’t be able to feed your baby while you have thrush, don’t be. It’s safe to continue nursing and feeding expressed milk while you are being treated for thrush. Similarly, using milk that was frozen while you had thrush is safe to feed your baby while you’re still being treated.
However, because freezing milk doesn’t kill the yeast, it’s possible your healthy baby could be reinfected. Avoid using breast milk that was expressed and frozen while you had thrush once you’ve completed treatment.
Finding What’s Right for You
Albee Baby is the oldest family-owned specialty baby shop in the US, and we pride ourselves on providing our customers with the best assortment of baby products anywhere, at fair prices, always. We’re committed to being an inclusive resource for parents and hope you feel empowered to find the right baby gear for your family. Still have questions? Feel free to contact our baby gear experts at 877.692.5233 or [email protected].

